Abstract

Introduction
Patients (pts) with relapsed/refractory (R/R) higher-risk myelodysplastic syndromes (MDS) have a dismal median overall survival (OS) of 4.3 - 5.6 months (mos) and a 1-year survival probability of 28% after failure of the 2 approved hypomethylating agents (HMAs) azacitidine (Aza), and decitabine (Dec). There is no existing standard of care for pts after failure of HMA therapy; hence, there is a critical need for effective therapeutic strategies. Venetoclax (Ven) is a selective, potent, oral BCL-2 inhibitor that in combination with Aza improved clinical outcomes as frontline therapy in pts with higher-risk MDS in an early phase clinical trial. We present an updated analysis of the safety and efficacy of Ven+Aza for the treatment of pts with R/R MDS.
Methods
This ongoing, phase 1b, open-label, multicenter study (NCT02966782) evaluated the safety and efficacy of either Ven monotherapy or Ven+Aza combination. Pts enrolled and treated with Ven+Aza were ≥18 yrs with R/R MDS and Eastern Cooperative Oncology Group performance status ≤2. Pts were considered R/R if they received a prior therapy with no response or had a response but subsequently relapsed after receiving at least 4 cycles of Aza or Dec within the last 5 yrs. Pts were excluded if they had myelodysplastic/myeloproliferative overlap neoplasms, had prior therapy with a BH3 mimetic, or underwent allogeneic hematopoietic stem cell or solid organ transplantation. For the Ven+Aza combination, pts were treated with escalating oral doses of Ven: 100, 200, or 400 mg daily for 14 days (d) every 28-d cycle. Aza was administered at 75 mg/m 2/d on 1─7 d every cycle. Responses were assessed per modified International Working Group 2006 criteria.
Results
Due to limited efficacy with Ven monotherapy, this analysis focuses on outcomes in pts treated with Ven+Aza combination only. As of April 30, 2021, 44 pts were treated with Ven+Aza (male 86%, median age 74 yrs [range 44-91]). Prior to enrollment, pts received a median of 1 HMA regimen and 65% of pts received >6 cycles of HMAs.
The median follow-up was 21.2 mos, range 0.4 ─ 37.5. Pts received a median of 4 cycles (range 1 ─ 32) of Ven treatment. Forty-two pts (96%) reported ≥3 grade treatment-emergent adverse events (AEs). The most common ≥3 grade hematological AEs were febrile neutropenia (34%), thrombocytopenia (32%), neutropenia (27%), and anemia (18%). Pneumonia (23%) was the most common ≥3 grade infection. Serious AEs were reported in 61%. There were 29 (66%) deaths, of which 1 (2%) occurred ≤30 d after the first Ven dose, and 3 (7%) occurred within ≤60 d of first dose. Nine (21%) deaths occurred due to disease progression, and 4 (9%) were due to AEs (gastrointestinal hemorrhage [n=1], and infections [n=3]). Twenty-one (48%) pts required Ven dose interruptions due to an AE, most frequently due to febrile neutropenia (n=7; 15%) and neutropenia (n=4; 9%). Five (11%) pts required dose duration reductions, and 9 (21%) pts required Ven discontinuation. Fifteen (34%) pts were alive at the time of data cutoff.
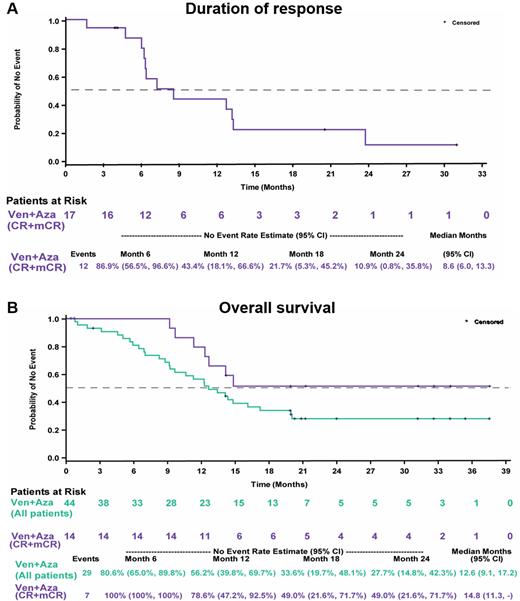
The objective response rate (mORR, defined as complete remission [CR] + marrow CR [mCR] + partial remission [PR]) rate was 38.6%, observed in 17 pts (CR 3, mCR 14, PR 0). Median time to first response of CR or mCR was 1.2 mos (range 0.7 ─ 6.3), and the duration of response for mORR was 8.6 mos (95% CI 6.0 ─ 13.3) (Fig A). Overall median progression-free survival was 8.6 mos (95% CI 5.4 ─ 14.3) and median OS was 12.6 mos (95% CI 9.1 ─ 17.2); mOS for pts with mORR was 14.8 mos (95% CI 11.3 ─ not estimable) (Fig B). Six pts with mCR also achieved hematological improvement. Post-baseline RBC and platelet transfusion independence (TI) was achieved by 16 (36%) pts overall with a median first duration of 4.0 mos (range 1.9 ─ 8.3). Nine pts (20.5%) moved to post-study transplant. Nine pts (20.5%) progressed to acute myeloid leukemia (AML). The median time to AML progression was 4.97 mos (range 0.03 ─ 19.84), and the median time to subsequent therapy was 5.7 mos (95% CI 4.8 ─ 8.8).
Conclusion
With longer follow-up, the tolerability and efficacy of the Ven+Aza combination in pts with R/R MDS were consistent with what was previously reported. In a very difficult-to-treat pt population, an ORR of 39%, RBC and platelet TI rate of 36%, and a median OS of 12.6 mos all suggest that Ven+Aza treatment leads to meaningful clinical benefits. Additional analyses, including associations of genetic mutations with clinical outcomes and patient-reported outcomes, will be presented.
Zeidan: Daiichi Sankyo: Consultancy; BeyondSpring: Consultancy; Kura: Consultancy, Other: Clinical Trial Committees; ADC Therapeutics: Research Funding; Amgen: Consultancy, Research Funding; Aprea: Consultancy, Research Funding; AbbVie: Consultancy, Other: Clinical Trial Committees, Research Funding; Geron: Other: Clinical Trial Committees; Agios: Consultancy; BioCryst: Other: Clinical Trial Committees; Genentech: Consultancy; Boehringer Ingelheim: Consultancy, Research Funding; Astellas: Consultancy; Astex: Research Funding; Pfizer: Other: Travel support, Research Funding; Jazz: Consultancy; Jasper: Consultancy; Ionis: Consultancy; Epizyme: Consultancy; AstraZeneca: Consultancy; Janssen: Consultancy; Gilead: Consultancy, Other: Clinical Trial Committees; Incyte: Consultancy, Research Funding; Novartis: Consultancy, Other: Clinical Trial Committees, Travel support, Research Funding; Loxo Oncology: Consultancy, Other: Clinical Trial Committees; Cardiff Oncology: Consultancy, Other: Travel support, Research Funding; Acceleron: Consultancy, Research Funding; BMS: Consultancy, Other: Clinical Trial Committees, Research Funding. Borate: Genentech: Membership on an entity's Board of Directors or advisory committees, Other: Advisory Board; Jazz Pharma: Research Funding; Daiichi-Sankyo: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; AbbVie: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees; Blueprint Medicine: Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees; incyte: Membership on an entity's Board of Directors or advisory committees, Research Funding; Rampal: Membership on an entity's Board of Directors or advisory committees; Galecto, Inc.: Consultancy; Promedior: Consultancy. Pollyea: Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: advisory board; Bristol Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees; Kiadis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Syndax: Honoraria, Membership on an entity's Board of Directors or advisory committees; Syros: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other; Teva: Research Funding; Curis, Servier: Other; Pfizer: Research Funding; Agios: Other, Research Funding; Karyopharm: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead: Consultancy, Honoraria, Other: advisory board; Astellas: Honoraria, Membership on an entity's Board of Directors or advisory committees; Foghorn: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Honoraria, Other: advisory board; Aprea: Honoraria, Membership on an entity's Board of Directors or advisory committees; Genentech: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Brunner: Celgene, Forty Seven Inc, Jazz: Other: Advisory Board; Novartis, Celgene, Takeda, AstraZeneca: Research Funding. Roncolato: AbbVie: Other: Investigator in AbbVie funded Clinical Trials. Garcia: AstraZeneca: Research Funding; Pfizer: Research Funding; Prelude: Research Funding; Genentech: Research Funding; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; Astellas: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding. Odenike: Celgene, Incyte, AstraZeneca, Astex, NS Pharma, AbbVie, Gilead, Janssen, Oncotherapy, Agios, CTI/Baxalta, Aprea: Research Funding; AbbVie, Celgene, Impact Biomedicines, Novartis, Taiho Oncology, Takeda: Consultancy. Watson: Astellas Pharma, Inc.: Consultancy; Roche, Amgen: Other: Travel support. Krishnadasan: AbbVie: Other: Investigator in AbbVie funded Clinical Trials. Bajel: Amgen: Speakers Bureau; Abbvie, Amgen, Novartis, Pfizer: Honoraria. Naqvi: Genentech/Roche: Current Employment, Current holder of stock options in a privately-held company. Zha: AbbVie: Current Employment, Current holder of stock options in a privately-held company. Hogdal: AbbVie: Current Employment, Current holder of stock options in a privately-held company. Zhou: AbbVie: Current Employment, Current holder of stock options in a privately-held company. Hoffman: AbbVie: Current Employment, Current holder of stock options in a privately-held company. Kye: AbbVie: Current Employment, Other: May hold equity.
Venetoclax is a BCL-2 inhibitor that is FDA approved for multiple indications. Venetoclax is not currently approved for the treatment of myelodysplastic syndrome. Azacitidine is FDA approved for continued treatment of adult patients with acute myeloid leukemia who achieved first complete remission or complete remission with incomplete blood count recovery following intensive induction chemotherapy and are not able to complete intensive curative therapy.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal